Patient-Driven Groupings Model (PDGM)
Every HHA is challenged with meeting the demands of the Patient-Driven Groupings Model (PDGM) especially as changes are consistently introduced. Winnolas powerful PDGM support provides the tools required to ensure success now and in the future. Updates in Winnolas are implemented, tested, and incorporated far in advance of any changes to PDGM affecting the HHA.
PDGM Overview
PDGM is the current Medicare payment methodology for home health agencies. Reimbursement is based on the patient’s characteristics and conditions. PDGM has four fundamental reimbursement components:
1. Admission Source and Episode Timing
2. Clinical Grouping
3. Functional Impairment Level
4. Comorbidity Adjustment
Payments under PDGM are two 30-day payment periods inside of a 60-day
certification period. PDGM utilizes 30-day payment periods categorized into
432 case-mix groups for adjusting the payment. Each of the 432 case-mix groups
has a specific LUPA threshold. CMS expects HHAs will schedule the number of visits
required to avoid a LUPA designation. The 30-day periods are placed into subgroups
of the following broad categories:
• Admission Source (From Claims)
Two Subgroups
1. Community
2. Institutional
• Episode Timing (From Claims)
Two Subgroups
1. Early
2. Late
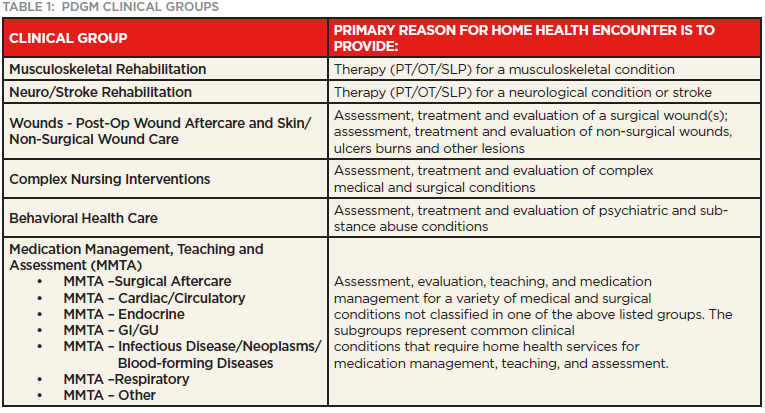
• Clinical Grouping (From Principal Diagnosis on Claim)
Twelve Subgroups
1. Musculoskeletal Rehabilitation
2. Neuro/Stroke Rehabilitation
3. Wounds
4. MMTA - Surgical Aftercare
5. MMTA - Cardiac and Circulatory
6. MMTA – Endocrine
7. MMTA - Gastrointestinal Tract & Genitourinary System
8. MMTA - Infectious Disease, Neoplasms, and Blood-Forming Diseases
9. MMTA – Respiratory
10. MMTA- Other
11. Behavioral Health
12. Complex Nursing Interventions
NOTE: MMTA - Medication Management, Teaching, Assessment
• Functional Impairment Level (From OASIS Items)
Three Subgroups
1. Low
2. Medium
3. High
• Comorbidity Adjustment (From Secondary Diagnosis on Claims)
Three Subgroups
1. None
2. Low
3. High
Total possible case-mix adjusted payment groups are 2*2*12*3*3 = 432.

Additional detail on each PDGM grouping category and adjustment to payments that are made within the PDGM.
Episode Timing
The first 30-day period is classified as early and all others are classified as late.
30-day periods continue until there is a gap of 60-days between the end of one 30-day
period and the start of the next. After a gap of 60-days, the next 30-day period is
classified as early.
Admission Source
Each 30-day period is classified into one of two admission source categories, community
or institutional, depending on what healthcare setting was utilized in the 14 days prior to
home health admission. Late 30-day periods are always classified as a community admission unless
there was an acute hospitalization in the 14 days prior to the late home health 30-day period.
A post-acute stay in the 14 days prior to a late home health 30-day period would not be classified
as an institutional admission unless the patient had been discharged from home health prior to
post-acute stay.
Clinical Grouping
The principal diagnosis provides the primary reason the patient is receiving home health services
under Medicare. When a new Episode is created, Winnolas checks that the Principal Diagnosis is valid
for PDGM and alerts the user if the diagnosis is invalid. This check ensures that the HHA’s provided
services
are eligible to receive payment. Each 30-day period is grouped into one of twelve clinical groups based
on
the patient’s principal diagnosis.
Functional Impairment Level
The patient’s functional impairment level is based on responses to 8 OASIS-D1
items for activities of daily living (ADL). The 8 OASIS-D1 items include: M1800 – 1840,
M1850, M1860 & M1033.
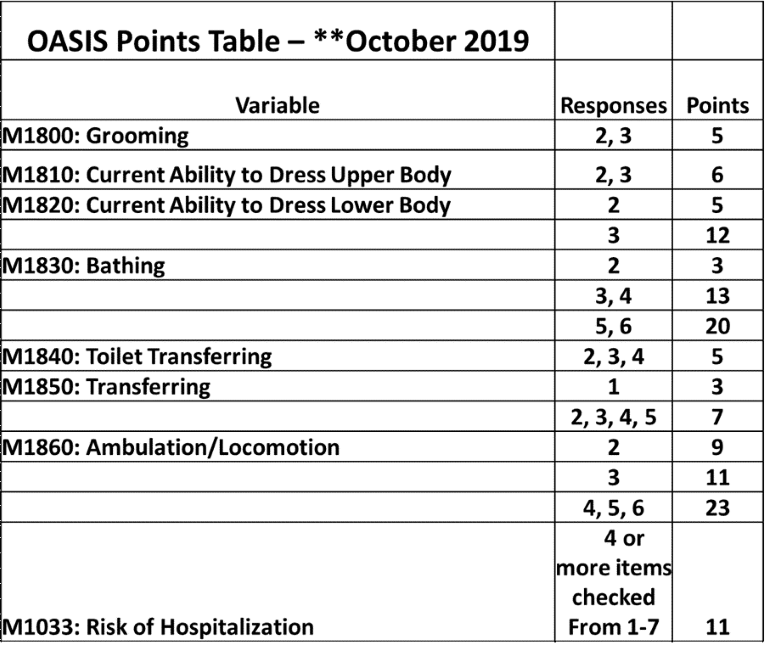
The patient is classified into one of three functional impairment levels:
1. Low
2. Medium
3. High
Oasis response for these M items has a different calculated weight toward the
rating scale used to determine that impairment level. While some responses contribute
points to the overall score of the functional impairment level, other responses do not
contribute.
Example:
M 1820 Patient’s current ability to safely dress lower body
Response 0 or 1
Response 2
Response 3
0 Points
6 Points
12 Points
Once the points are calculated from the above table, the total points are taken to the next step of determining the level of impairment dependent on the Clinical Category. This is the ONLY area of the PDGM case-mix calculation that will be taken from the OASIS documentation.
Comorbidity Adjustment
Comorbidity is the presence of one or more disease processes or disorders in the same person. Two or more diseases that interact in a way that requires those numbers of a care team to take into consideration both diseases and disorders in the treatment plan. Comorbidities and their identification in a patient’s plan of care are one of the building blocks under PDGM and are considered when determining the resources needed to care for that patient.
The PDGM includes a comorbidity adjustment category based on the presence of secondary diagnoses. A 30-day period may receive no comorbidity adjustment, a low comorbidity adjustment, or a high comorbidity adjustment.
Adjustment Levels
NONE:
LOW:
HIGH:
No comorbid diagnosis that qualify for the adjustments
There is a reported secondary diagnosis that is associated with higher resource use.
There are two or more secondary diagnoses that are associated with higher resource use when reported together
A 30-day period can have a low comorbidity adjustment or a high comorbidity
adjustment, but not both. If a 30-day home health period of care does not have
reported comorbidities that fall into the low or high adjustment levels, no comorbidity
adjustment is applied.
Determining Case-Mix Weights for PDGM
The case-mix weight for each of the 432 different payment groups under the PDGM are determined by dividing the predicted resource use for each PDGM payment group by the overall average resource use of all 30-day periods and are then used to adjust the 30-day payment rate.
Costs are determined using a Cost per Minute plus Non-Routine Supplies approach, and the case-mix
weight reflects each group’s predicted mean cost relative to the overall average.
• Case-mix weights are used to adjust the base payment amount
• Higher resource need periods have a higher case-mix weight and receive
a higher payment adjustment
• CMS provides an annual recalibration of the PDGM case-mix weights to reflect
the most recent utilization data
Additional Payment Adjustments for PDGM
Low Utilization Payment Adjustment (LUPA) Threshold
Each of the 432 case-mix groups has a threshold to determine if the period of care would receive a LUPA. Currently, the LUPA threshold ranges between 2 and 6 visits. A RAP is not required for LUPA periods of care; however, it is more challenging to predict when a period of care will result in a LUPA since it’s basedon variable thresholds.
If the HHA provides fewer than the threshold of visits specified for the period’s HHRG, they will be paid a LUPA, instead of a case-mix adjusted payment for a 30-day period of care. CMS expects HHAs will schedule the number of visits required to avoid a LUPA designation.
Outlier Payments
When a 30-day period of care involves an unusually large number or a costly mix of visits, the HHA may be eligible for an additional outlier payment. Once the imputed cost of a 30-day period of care exceeds a threshold amount, the HHA receives a payment equal to 80 percent of the difference between the imputed costs and the threshold amount.
Payments would be adjusted if a beneficiary transfers from one home health agency to another or is discharged and readmitted to the same agency within 30 days of the original 30-day period start date. The case-mix adjusted payment for 30-day periods of that type is pro-rated based on the length of the 30-day period ending in transfer or discharge and readmission, resulting in a partial period payment.
Conclusion
Winnolas understands PDGM and the challenges HHAs face in remaining compliant, efficient, and successful. Our staff is prepared to support PDGM for your HHA now and in all future developments. Let Winnolas bring peace of mind to your HHA by providing consistent updates to keep up with all the changes in PDGM long before they become a requirement.
Winnolas PDGM Powerful Features
• PDGM Valid Principal Diagnosis
When a new Episode is created, Winnolas checks that the Principal Diagnosis is valid for PDGM and alerts the if the diagnosis is invalid. This check ensures that the HHA’s provided services are eligible to receive payment.
• PDGM Case Mix Analysis ReportsContains all the details for the 1st and 2nd 30-day payments including the final payment impact to the agency based on the HIPPS code generated by the OASIS.
• PDGM PricerFor each 30-day payment period, the HHA enters their cost of services provided to accurately determine their Profit/Loss based on the final PDGM payment.